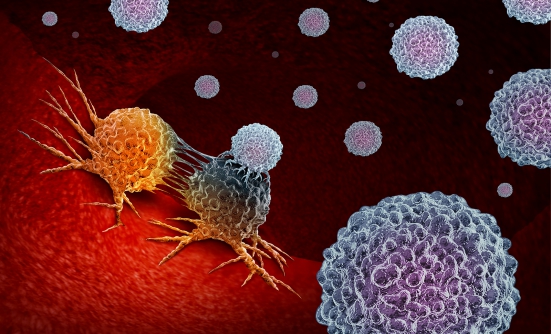
After many years in development, the newest type of immunotherapy known as CAR T-cell therapy (or gene therapy) is becoming a mainstream treatment in some types of blood cancer, specifically for leukemia and lymphoma so far. CAR T-cell therapy involves modifying the patient’s own immune cells, called “T-cells,” to enable them to attack cancer cells.
The first CAR T-cell therapy to become available in the United States was Kymriah (tisagenlecleucel), which was first approved by the FDA in August 2017 for patients younger than age 25 for acute lymphoblastic leukemia, or ALL. A few months later, in May 2018, the FDA approved Kymriah for adults with a type of lymphoma called large B-cell lymphoma.
The second CAR T-cell therapy, Yescarta (axicabtagene ciloleucel), was approved by the FDA in October 2017 for adults with several types of B-cell lymphoma, including relapsed (returning) or refractory (not responding to therapy) diffuse large B-cell lymphoma (or DLBCL), high-grade B-cell lymphoma, and DLBCL from follicular lymphoma.
The introduction of CAR T-cell therapies last year was met with great enthusiasm by cancer experts as a new way to fight cancer.
“The approval of Yescarta brings this innovative class of CAR T-cell therapies to an additional group of cancer patients with few other options,” said Peter Marks, MD, PhD, Director of the FDA’s Center for Biologics Evaluation and Research.1
At the 2018 National Comprehensive Cancer Network Hematologic Malignancies Congress, Frederick L. Locke, MD, Program Co-Leader, Immunology, at Moffitt Cancer Center in Tampa, Florida, said that a third CAR T-cell drug is close to being submitted for FDA approval, and many other CAR T-cell drugs are now in clinical trials.
“About 750 cell therapies are in development, and about half are CAR T-cells,” Dr. Locke said. For now, CAR T-cell therapies are used in patients whose lymphoma or leukemia does not respond to other treatments. However, “The next advance will be earlier use of these therapies,” Dr. Locke predicted.
He explained that the first responses to CAR T-cell therapy were reported about 8 years ago and were quite dramatic in a few children and adults with leukemia, who had no other treatment options. Their responses lasted a long time, and a few of those first patients had no sign of disease after treatment with a CAR T-cell therapy.
In an interview with CONQUER magazine, Gwen Nichols, MD, Chief Medical Officer at the Leukemia & Lymphoma Society, said, “Because this breakthrough is so new, doctors are very excited about the potential of this therapy, but the patients need to understand what the current data are regarding how long they are likely to stay in remission after this therapy.”
How CAR T-Cell Therapy Works
To create a CAR T-cell therapy, scientists collect (or harvest) T-cells from the patient and send them to a lab. There, the cells are genetically engineered to create the CAR protein on the surface of the cells. These CAR proteins allow T-cells to recognize a specific antigen, such as CD19, on the cancer cells. The engineered T-cells are then reinfused back into the patient’s blood. CAR T-cells are typically delivered in the hospital. Currently, it takes approximately 3 weeks to manufacture CAR T-cells.
“It takes many weeks to harvest cells, prepare them, multiply them, freeze them, and send them back,” according to Dr. Nichols. “The current process is expensive and requires many steps, so one aspect of CAR T-cell therapy that patients need to consider is whether they can afford the time necessary for this treatment process.”
Key Side Effects
The main severe side effects with CAR T-cell therapy include cytokine release syndrome and neurologic side effects. Severe adverse effects of CAR T-cell therapy are managed by immunosuppression. Cytokine release syndrome develops as a reaction to the engineered T-cells being infused into the patient with CAR T-cell therapy.
On the day the FDA approved the first CAR T-cell therapy (Kymriah) in August 2017, it also approved the new drug Actemra (tocilizumab) for the treatment of cytokine release syndrome caused by a CAR T-cell therapy. For severe cases, Actemra is used with corticosteroids, to reduce the likelihood that the syndrome will progress. Patients continue to respond to CAR T-cell therapy while they are receiving Actemra.
“We feel confident that we can treat early, and they [patients] will respond and benefit from CAR T-cells,” Dr. Locke said. “It took 30 years to develop CAR T-cells. But with second-generation CAR T-cell therapy, the field has rapidly advanced, and now we give this as standard of care.” He added that in 2018, the American Society of Clinical Oncology named CAR T-cell immunotherapy as the main advance of the previous year.
Other serious side effects with CAR T-cell therapy are neurologic problems, such as confusion, seizures, or severe headaches. According to Dr. Nichols, “An adverse reaction to the treatment can cause patients to be in the intensive care unit for a day or 2 during treatment. For a very sick patient, that can be the straw that breaks the camel’s back.”
Clinical Trials
The results in clinical trials of CAR T-cell therapies in aggressive B-cell lymphoma and in multiple myeloma are encouraging, Dr. Locke says. Many clinical trials are studying new CAR T-cell therapies, which will likely lead to new drugs in the near future for other types of cancer, especially multiple myeloma.
The availability of CAR T-cell therapies means long periods without signs of cancer for some patients and potentially bringing a cure for others. However, understanding why some patients are not responding to these treatments is now the main challenge for researchers. A main goal for researchers now is uncovering the reasons why the same disease responds to treatment in one patient but not in another.
Patients whose cancer is not responding to current treatment may benefit from talking with their care team to find out if they are a good fit for a specific CAR T-cell clinical trial.
Key Points
- CAR T-cell therapy is now considered a standard of care for some patients with leukemia or lymphoma
- The main severe adverse events with CAR T-cell therapies are cytokine release syndrome and neurologic problems
Reference
1. US Food and Drug Administration. FDA approves tisagenlecleucel for adults with relapsed or refractory large B-cell lymphoma. May 1, 2018. www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm606540.htm.
Patient Resources
American Cancer Society
www.cancer.org/treatment/treatments-and-side-effects/treatment-types/immunotherapy/car-t-cell1.html
National Cancer Institute
www.cancer.gov/about-cancer/treatment/research/car-t-cells