
As a software sales professional for 35 years and a student of behavioral sciences, I learned how to communicate by interpreting body language with my customers. This skill became invaluable to me during my “Covid Cancer” journey.
Body Language
My experience with stage III breast cancer began with a monthly breast exam, when I found a lump. It felt like a fibroid, so I monitored it. When the lump didn’t decrease in size, I scheduled an appointment with my primary care doctor. Even with a mask, I could hear the concern in his voice and felt him squeeze my shoulder, so I knew this wasn’t just a fibroid. But when he scheduled tests at the hospital for that same day and said, “We’ll get you through this,” I knew this was serious.
Four lab tests, 3 doctors, and 5 hours later, I was rapidly becoming a body language expert. I had to interpret masked technicians’ eyes, nurses’ mannerisms, and identify the incongruity of what the doctors’ voices said with what was left unsaid.
Behind a Mask
As humans, we usually depend on seeing the entire face plus a person’s body language to fully interpret what is being said. This process is challenging behind a COVID-19 mask and is extra difficult to decipher behind a double mask and a face shield. No one used the word “cancer” with me, yet every single member of my healthcare team’s body language implied a serious diagnosis.
So, my senses were on high alert when the doctor was reviewing my tests. I asked him, “I know you can’t use the cancer word for certain, but if I were your wife or daughter or sister, what would you tell me?”
He responded, “As soon as the hospital doors close behind you, call this breast surgeon and get his first available appointment.” I was glad I had the guts to ask the question, but scared by what his recommendation implied.
Invasive Lobular Carcinoma
Within 7 days, I had a breast biopsy, a 3D mammogram, blood tests, an ultrasound, and an x-ray. Within 2 weeks, I also had an MRI, an additional mammogram, an EKG, a bone density test, a CT scan, more blood work, and a COVID-19 test to prep for surgery. After the biopsy, my diagnosis was stage II (early-stage) invasive lobular carcinoma.
A modified mastectomy, sentinel lymph node removal, and plastic surgery were scheduled. I was told that my odds were up to 86% chance of survival to the 5-year mark. In surgery, they found that the tumor was 2 cm bigger than it had appeared on the mammogram and ultrasound.
The cancer had also spread to one of the lymph nodes. I realized that this was bad news when the highly efficient and matter-of-fact breast surgeon furrowed his brow and patted my knee, while giving me the bad news that I had stage III disease, meaning advanced cancer.
My odds of survival to the 5-year mark decreased by 12%. As a result, I was scheduled for 16 chemotherapy treatments over 20 weeks, 7 weeks of daily radiation, and further surgery.
COVID-19 Solo Act
My husband would drive me for each doctor visit or lab test, then drop me off, saying, “Be courageous,” and give me a hug. Then I’d mask up and go through each of the clinical processes alone. This sense of loneliness during each clinical interaction was as challenging as the tests themselves.
Because of COVID-19, registering for a procedure, having an exam, or a lab test were dehumanizingly clinical. Because no one could join me, the testing process was very lonely. I began to feel like a number while at the hospital or the doctor’s office. Rarely did anyone make eye contact with another patient or with a healthcare worker. The tests were perfunctory, and no human touch was involved, unless necessary for the test. This entire testing process is dehumanizing enough without COVID-19. With it, every appointment was a solo act, and as a result, each test was sterile and mechanical.
By July 2020, COVID-19 was raging. As I read news articles, I realized that my healthcare providers were exhausted physically and mentally. They had undoubtedly lost patients, and maybe colleagues. Their natural instincts were probably to remove themselves emotionally from their patients, to safeguard their emotions.
But patients like me, amid “Covid and Cancer,” crave human interaction. I realized that I had to do something to make this experience more bearable.
Power Through Connecting
First, I decided to get to know other patients in the waiting room. I began with small talk. Even when the patients never looked up, I could get about half of them to begin to chat with me. This helped improve our spirits, as we realized that we were not alone in this journey.
Second, I began to reach out to the healthcare workers. For example, when meeting with an admitting nurse, I would try to find something on the desk or wall to begin a personal conversation. With the technicians performing tests, I would point out the embarrassing situation and make light of it, so the nurse would realize I was a human, not just another test subject. With doctors and nurses, I’d ask about their family, and get them to tell me how challenging remote learning was for their kids.
Slowly, I began conversing with other patients and healthcare workers. Often, when I saw the same technician or nurse a second or third time, I’d bring up the earlier conversation to reconnect with them quickly.
The more I reached out, the less threatening and lonely my waiting, exams, and tests became. Soon, I began to feel a connection to patients and healthcare workers, and my feelings of isolation began to fade. I was still quarantining at home, but lab work, doctor visits, and hospital tests became something to look forward to, as the people administering them became my human lifelines.
My Chemo Team
But I still had to get through treatment. I endured the very challenging chemotherapy regimen with sheer personal tenacity, spawned on by the encouragement of the team administering the chemotherapy. You are not allowed to work as a doctor, nurse, or technician in the infusion suite unless you have an outgoing and upbeat personality. That is a great thing! The chemotherapy team’s positive attitudes made a huge difference to me. Similarly, connecting with other patients each week gave me the encouragement to endure the painful 20-week course of chemotherapy.
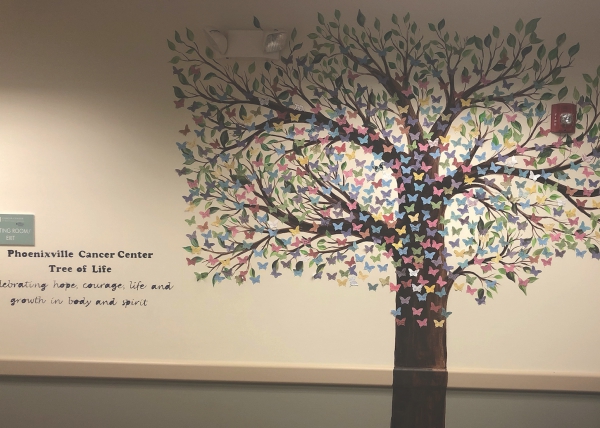
The Tree of Life
At the Cancer Center, Phoenixville Hospital Tower Health, in Phoenixville, Pennsylvania, where I received my treatment, all patients who receive chemotherapy can add a butterfly to the “Tree of Life” after their last infusion. This symbolizes movement from being a patient to being a cancer survivor.
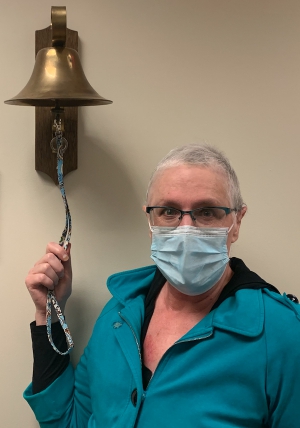
The highlight of my chemo experience was when my favorite oncology nurse encouraged me to put a butterfly on the chemo tree, demonstrating the completion of my course of chemo. My nurse then gave me a “Covid hug,” in which you hug each other with a clean blanket between you.
I left the treatment center that day weeping with pride for completing the treatment. I felt I had run a marathon for 20 weeks, with the chemo team sprinting alongside me. Although tired, weak, and immunosuppressed, I completed this difficult course of chemotherapy and my spirits were very positive.
Signs of Humanity
I’m now entering the next stage of treatment: 7 weeks of radiation, followed by reconstructive surgery. Regardless of the outcome, I will be forever grateful for the humanity of my entire healthcare team when they showed me an empathetic voice, shared a personal story, gave me a pat on the shoulder or squeezed my knee, and looked me directly in the eyes while undergoing treatment.
These signs of humanity broke down the COVID-19 barriers of double masks, face shields, and gloves, while enabling me, the patient, to feel like a human being.
If you or your loved one is undergoing a cancer journey during COVID-19, remember to find a team of healthcare professionals who are highly skilled in beating cancer, but also willing to deliver a little compassion along the way.
If you are a cancer survivor, seek out opportunities to connect with other patients and with your entire healthcare team. Your spirits will appreciate these human efforts amid the dehumanized experience of COVID-19 and cancer. Remember that your human connections are important in finding the will and endurance to beat cancer during the COVID-19 pandemic.
Editor's Note
An earlier version of this article had a wrong name for the cancer center.















