It’s been more than a year and a half since the COVID-19 pandemic began, creating massive interruptions to our daily lives that we’re still experiencing today, as the delta variant continues to spread. But for me, the beginning of the COVID-19 pandemic marked a different kind of change: it meant a complete upheaval of potentially lifesaving treatment for a rare form of cancer I’ve been diagnosed with.
Wrong Diagnosis
In October 2017, when I was 68 years old, I went to my local emergency room in Wilmington, North Carolina, in the middle of the night with intense pain in my abdomen. After a long wait and a variety of tests, I was told that I likely had pancreatic cancer, a devastating diagnosis with few treatment options.
But after additional testing, it was determined that my original diagnosis was incorrect, and that I had stage IV adenocarcinoma of the abdomen, or stomach cancer.
My daughter lives in Columbus, Ohio, and had a connection to the Ohio State University Comprehensive Cancer Center (OSUCCC)–Arthur G. James Cancer Hospital and Richard J. Solove Research Institute, a National Cancer Institute (NCI)-designated comprehensive cancer center. At the urging of my family, I went there for a second opinion.
The good news was: I had genetic testing that revealed my cancer involved the RET fusion and FGFR mutations (different types of gene alterations) that caused my cancer. The bad news was: at that time, there was no drug that was able to specifically target these gene alterations.
So I returned to North Carolina and started intense chemotherapy. The cancer was in remission, briefly, but then it came back. I then had radiation, but again the cancer came back.
Clinical Trial and Second Chances
My local oncologist contacted the OSUCCC, and this time I was eligible to join a new program. I qualified for a clinical trial of a recent oral therapy that had been previously approved for leukemia but was now investigated in solid tumors. The drug is called Iclusig (ponatinib), and it targets my specific genomic alterations, the RET fusion and FGFR mutation, among other genetic alterations.
The study has been led by Sameek Roychowdhury, MD, PhD, an oncologist at that NCI-designated comprehensive cancer center in Ohio. This clinical trial is continuing, and it has given me a chance to fight my cancer, which didn’t seem possible just a few weeks before I joined it.
There was, however, one catch: I would need to commute all the way from North Carolina to Columbus, Ohio, for the treatment, which is a 10-hour drive each way, and I would need to make the trip every 4 weeks, so I could be evaluated in person by doctors. This was a huge commitment, but ultimately it was an easy decision.
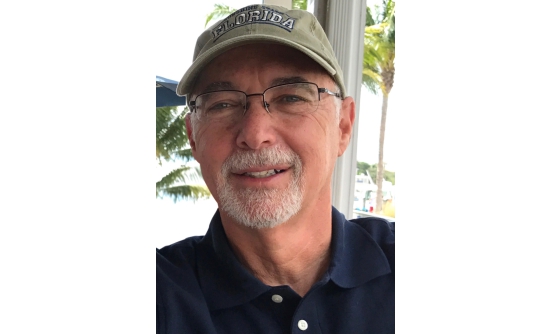
And it was worth it! The drug worked. I have been symptom-free since 2018. I take 2 pills of Iclusig a day, and I stay active by lifting weights and exercising. Although I’m 72 and retired, I work part time as an auto transporter, moving cars in the tristate area for local car dealerships. I’m happy to keep moving, and my doctors encourage me to keep busy and active.
And Then…
So everything was working out fine. Then the COVID-19 pandemic hit. Suddenly, my plans were much more complicated than a 10-hour drive several times a year.
At first, we had to figure out the logistical challenges. Lockdowns meant that a lengthy trip across several states was not possible, and I wondered whether I would be able to continue my important clinical trial, as travel became restricted.
For me, that uncertainty was as scary as any of the pandemic news. Thankfully, they figured out how to move my clinical trial to telemedicine, which allowed me to continue treatment. Instead of making the trip, I got my lab tests, CT scans, and electrocardiogram tests that were needed for participation in the clinical trial close to home, and my medications were mailed to me.
To my surprise, I loved it. It allowed me to skip the long drives, stay close to home, and receive the same level of care. I did video chats with Dr. Roychowdhury to review my test results and ensure that things were progressing well, and suddenly I had several extra hours in the month that I was not spending on the road.
But that was only a temporary change. After a few months, nationwide policy changes meant that I had to return to my trips. However, the cancer center worked with me to cut down on my trips, and now I’m only traveling to Ohio once every 8 weeks, a welcome change.
Another Layer
In addition to the disruption of my routine, however, the pandemic added a new layer to my treatment; it was a truly scary time to have cancer. During “normal” times, receiving treatment for life-threatening cancer was hard. During the pandemic, it became even harder, and more dangerous.
I was used to being scared of the cancer I knew I had. I wasn’t used to being scared of an invisible disease infecting millions of people around the world. At times, I was so nervous that I had difficulty falling asleep.
But I managed to make it through, thanks in part to the excellent team at OSUCCC. As infection cases dropped this year, my path to Ohio every couple of months started to look a bit less daunting, especially after getting fully vaccinated earlier this year (2021).
Telemedicine for Clinical Trials
I hope that my experience, and the experiences of others during this pandemic, can help to inform future medical policy. The brief exposure I had to telemedicine was eye-opening for me, revealing the impact that virtual care can have on patients like me.
I’ve been fortunate to avoid compromising situations, and Ohio has been very careful not to put anyone at risk, but a 10-hour trip each direction can present its own risks. Dr. Roychowdhury is also an advocate for expanding telemedicine for clinical trials.
Get A Second Opinion
I also hope that my story helps patients with cancer to realize the importance of getting a second opinion. Who knows where I would be today without the doctors in Ohio who connected me with the clinical trial that’s provided the right treatment for my cancer. Ponatinib is still not approved for patients with stomach cancer, and the only way for me to receive it was in a clinical trial.
To people who are fighting cancer themselves, or those who are helping a loved one battle cancer, remember to keep going. Even with the odds stacked against you in a global pandemic, it’s worth the fight.